Conditional Reprogramming: A Novel Way to Study the Novel Coronavirus
Posted in GUMC Stories | Tagged 2019 Novel Coronavirus, biomedical research, Center for Cell Reprogramming, COVID-19, global health, SARS-CoV-2
(July 8, 2020) — Even during the early days of the pandemic, it was apparent that some patients with COVID-19 develop multisystem problems in addition to respiratory infections. Specifically, the virus can cause life-threatening gastrointestinal, cardiac, neurological and renal complications. These severe cases appear to occur because the virus rapidly replicates in various organs, causing an immune response that worsens inflammation and hampers recovery.
The Key to Invasion
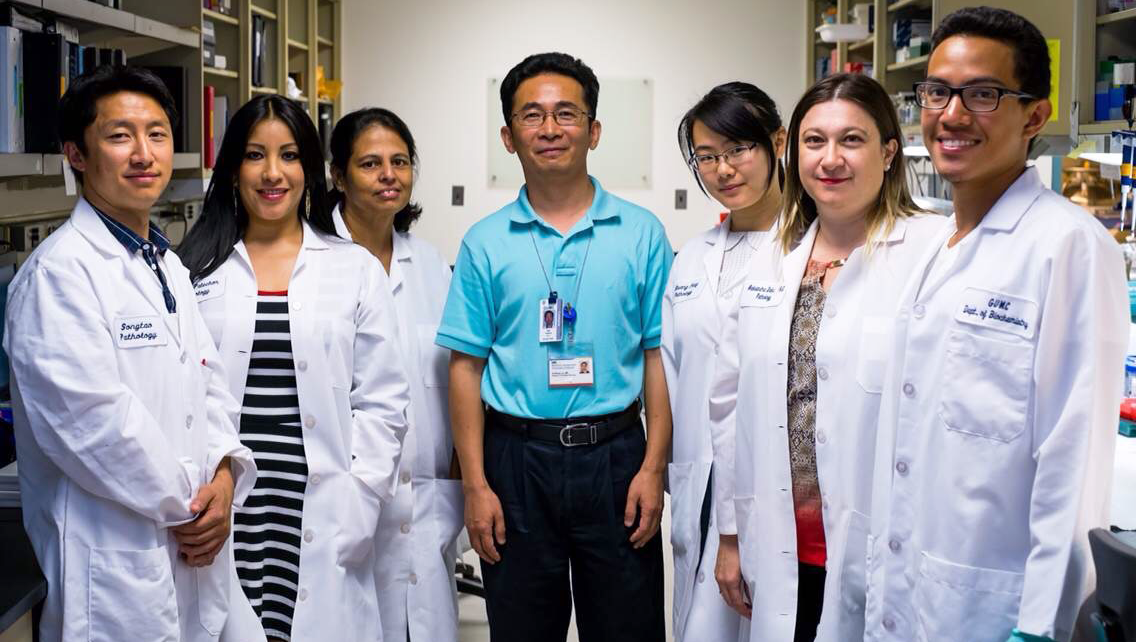
For Xuefeng Liu, MD, professor of pathology and oncology, figuring out how the coronavirus enters healthy cells and blocking that mechanism with antiviral drugs could be the key to mitigating the disease course. To further this investigation, he was awarded one of the 15 COVID-19 pilot research grants from Georgetown University Medical Center in April.
It turns out that SARS-CoV, the virus that caused SARS and the resulting global outbreak in 2003, and SARS-CoV-2, the virus that causes COVID-19, both rely on the ACE2 receptor to gain entry into cells. ACE2, or angiotensin-converting enzyme 2, is a protein that is present in cells that line the inside of blood vessels of many organs. Other cell surface proteins also play a role in facilitating the invasion of the virus into host cells.
Unique Challenges
Liu says that there are several limitations to using current cell lines and animal models to study the novel coronavirus. “Current cell lines are almost all abnormal cells, either from animal or human cancers,” he says. “Battles between these cells and the virus are very different from normal cells, and the latter are very difficult to culture in the lab.” He explains that animal models are important, but there can be very different interactions between the virus and these hosts, making it difficult to generalize about what is happening in humans.
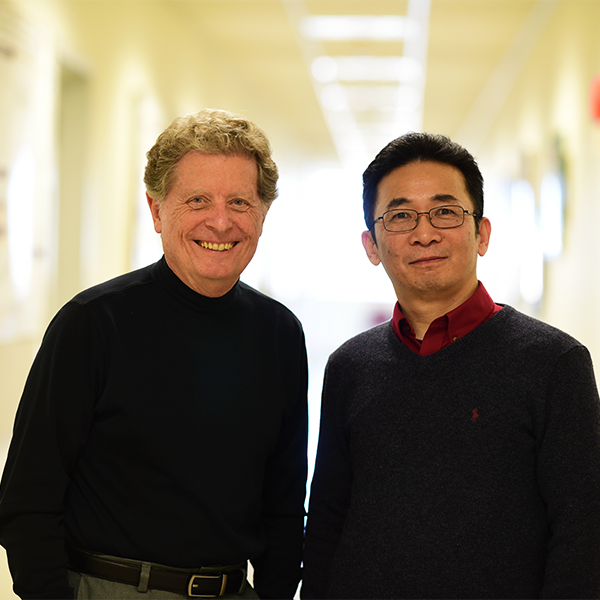
To overcome these challenges, Liu is using conditional reprogramming (CR) to grow the cells in the lab. He and Richard Schlegel, MD, PhD, professor and chair of the department of pathology, first described this revolutionary technique in 2011. Liu and Schlegel co-direct the Center for Cell Reprogramming and have used CR to extensively study cancer cells and targeted therapies. CR allows cells to be grown quickly and indefinitely without the limitations of other cell lines that often malfunction, so that they become “immortal.” These cells mimic the physiological conditions of cells or tissues in the human body. “We will use CR and a special in vitro culturing system to proliferate lung, trachea and nasal cavity cells so we can determine how the virus enters and damages these cells, and how these cells attempt to fight the virus,” Liu says.
Next Steps
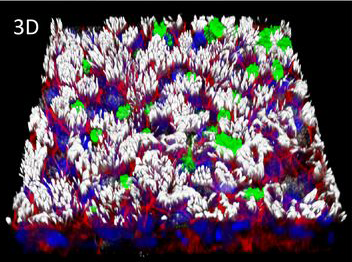
One of the most exciting outcomes from this work will be determining whether drugs can block the virus from entering cells and how drugs prevent cell damage by the virus. In his study, Liu plans to test over 500 antiviral compounds.
A striking occurrence during the pandemic is how COVID-19 has disproportionately affected racial/ethnic minorities and underserved groups, especially African American, Latinx and Native American communities in the U.S. “We’ve conditionally reprogrammed cells from diverse groups of individuals that we hope will provide direct biological evidence to help explain these disparities,” Liu says. “For example, there may be differences in expression of viral receptors in host cells. This type of finding could lead to novel interventions and provide a more individualized approach to prevention or treatment.”
Although it is difficult to imagine dealing with more viral threats, Liu says that these types of advances in the laboratory will be key to combating the potential morbidity and mortality that affected individuals may face in the future.
Beth N. Peshkin
GUMC Communications
Georgetown University has several issued patents and patent applications in U.S. and foreign countries for conditional cell reprogramming technology. The technology is licensed exclusively to a company for further development and commercialization. Georgetown University and the inventors (Liu and Schlegel) receive payments and potential royalties from commercialization of the licensed technology. Schlegel is also a co-founder in the company that has a license to this technology.
