Surgeon and Basic Scientists Partner to Develop New Way to Suss Out Early Problems in Liver Transplantation
Posted in GUMC Stories | Tagged liquid biopsy, liver transplant, organ transplant, research, translational research, transplant rejection
(June 25, 2024) — A liver transplant can be a lifesaving procedure for people with decompensated cirrhosis, some cancers and acute liver failure, but there are many potential complications: from infection, to problems with the bile ducts, to organ rejection. Continued monitoring is vital so that doctors can catch problems early and intervene.

Now, a unique collaboration between basic scientists at Georgetown University Medical Center and a transplant surgeon at MedStar Health could change how and when problems are identified, leading to expedited treatment and significantly reducing the need for additional expensive and invasive testing.
The primary tools currently used for monitoring the health of a transplant are blood tests and imaging studies, which can give doctors a warning signal that something is going wrong. However, these tests often offer little additional information about what’s actually triggering the trouble. As a result, patients have to undergo multiple follow-up tests and invasive tissue biopsies to determine if there is a rejection or another source of the problem.
The Georgetown-MedStar Health collaborators have uncovered a new way to both pick up the warning signal and identify exactly where the problem is in the liver by identifying fragments of DNA from dying liver cells that circulate in the bloodstream. The “liquid biopsy” could potentially detect problems as early as the second week after a transplant.
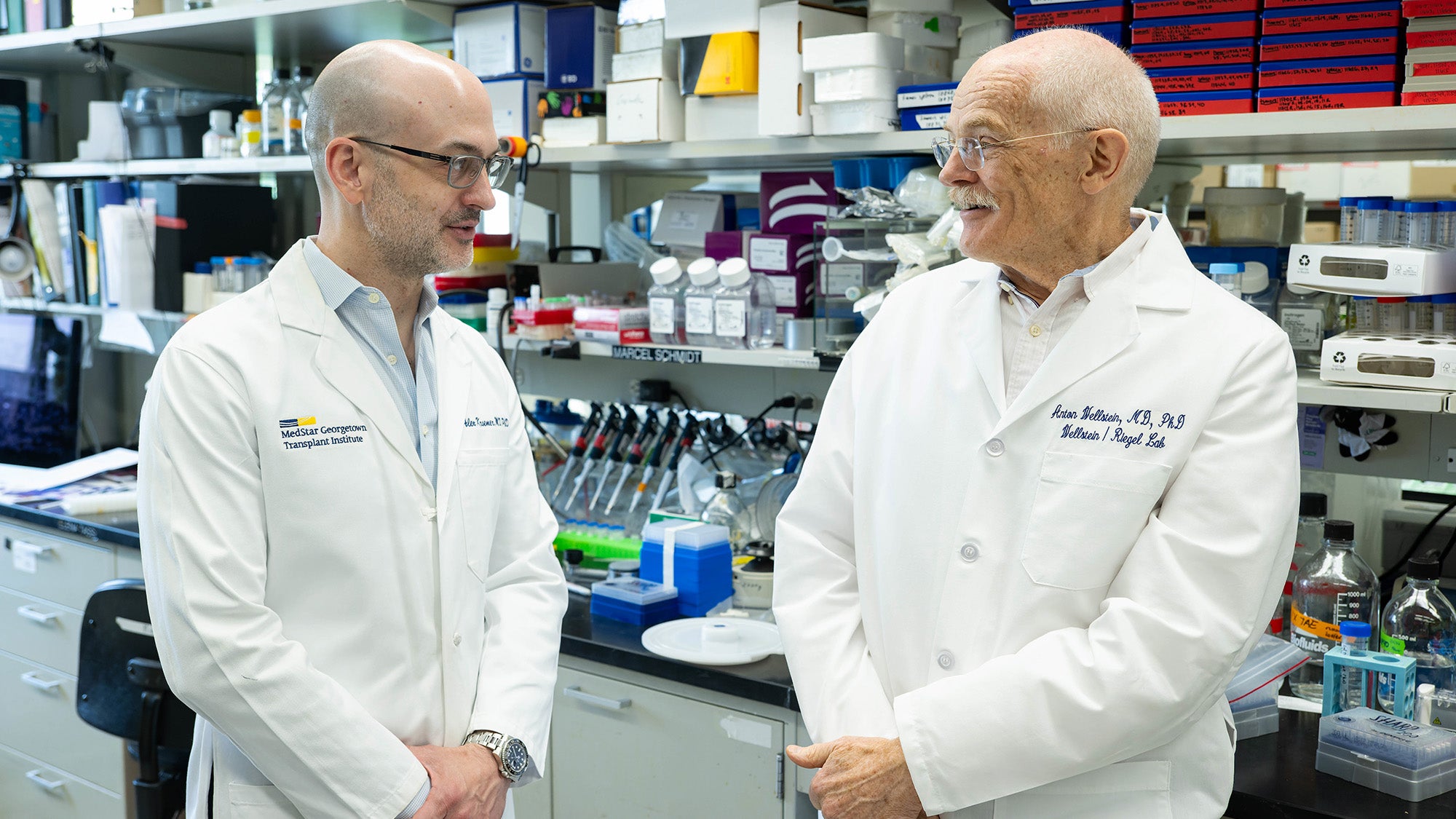
“This is a really big step forward,” said Anton Wellstein, MD, PhD, professor of oncology and pharmacology at Georgetown’s Lombardi Comprehensive Cancer Center, and a co-author of a study currently in preprint that describes the process. “It’s something that has never been done before, and it’s a very exciting result.”
Tracing Genetic Fingerprints
When a cell dies and disintegrates, some of the debris washes away into the bloodstream, where it circulates through the body.
Scientists have long been able to use genetic testing to determine if parts of dead cells in a patient’s bloodstream are coming from their own body or from their donated liver. But the technology has major limitations, Wellstein said.
“All you will find out is that there is damage, but you don’t know where the damage is from,” he explained.
The new work builds on an understanding of how cells differentiate, or develop into different types. During differentiation, a chemical modification called DNA methylation controls certain genes on the differentiated cell’s strands of DNA, leaving behind a chemical signature — a genetic fingerprint.
“That means the DNA fragments from dying cells that we find in the bloodstream carry a fingerprint of their cell of origin — like a ZIP code,” he said.
Pinpointing a Liver Tissue Failure
For the first phase of their work, researchers built a “library” of these fragments, called cell-free methylated DNA, and identified the methylation pattern for each cell type, said Alex Kroemer, MD, PhD, a transplant surgeon at MedStar Georgetown University Hospital and director of the Center for Translational Transplant Medicine at Georgetown University Medical Center.
“Hepatocytes, cholangiocytes, endothelial cells,” he said. “Basically, a whole-body map of distinct, relevant cell types, even beyond the liver, was established, so we’d actually know what we’re measuring.”
The second phase of their work involved testing blood samples from liver transplant patients at regular intervals and following their outcomes. Researchers analyzed 135 blood samples collected from 44 volunteer patients both before and after transplant.
The samples showed that cellular damage occurs across multiple tissue types immediately after transplant, but that the graft — or transplanted tissue — begins to stabilize within the first week. After that point, the team found that elevated levels of certain DNA fragments indicated early signs of a graft injury. Significantly, researchers also showed that they could use the chemical signature of the methylated DNA fragments to determine the cellular location of the injury.
A Path to Personalized Care
The discovery could lead to several significant advances for liver transplant patients, beginning with faster diagnosis of transplanted tissue rejection for more focused care.
“If you were to know, for instance, that the biliary compartment [of the liver] is injured but not the hepatocellular compartment, you could provide a more personalized treatment approach that leads to better care for the patient,” Kroemer said.
In addition to being faster and less invasive than a traditional tissue biopsy, the blood test is also potentially more accurate, he added. “With biopsies, there’s always the potential for sampling bias, because you’re not sampling the whole liver,” he said. “It’s just one small core that’s being evaluated.”
A liquid biopsy could also be used to monitor treatment for specific issues. For example, if a patient is being treated for organ rejection, blood tests given at regular intervals could tell doctors if the therapy is working, or if a different approach is needed.
Finally, Kroemer noted, the study found that the test could detect early signs of poor outcomes — long before they became acute.

“There may be a predictive element, which was quite surprising,” he said.
It’s possible the technology could even be used in the future to assess donated livers for their viability and risk of poor outcomes, he said.
The team’s work, “Circulating, Cell-Free Methylated DNA Reveals Cellular Sources of Graft Injury After Liver Transplant,” was recently presented by first author Megan McNamara, a Georgetown MD/PhD student, at the 13th International Symposium on Circulating Nucleic Acids in Plasma and Serum in Graz, Austria. McNamara was awarded the Michael Speicher Prize for best presentation. The research was also selected for a prestigious plenary presentation by McNamara at a recent NIH conference, New Frontiers in Liquid Biopsies.
McNamara said the results were exciting, and that she was gratified to see the study receiving such significant recognition.
“I was thrilled by the positive reception of our work,” she said. “It meant a lot to me, and it speaks to the innovation and the potential impact of this work in the field.”
Researchers are moving forward to find a partner to help commercialize the technology and develop it for clinical use, Wellstein said. At the same time, the team is continuing to dive deeper to identify more subtypes of liver cells for more precise diagnoses, as well as applying the technology to organs beyond the liver.
“The research is never finished,” he said. “This is the initial step on a long road.”
Georgetown University filed a patent application with the USPTO and other jurisdictions related to some of the approaches described in this story. Wellstein, Kroemer and McNamara are named as co-inventors on this application.
