Inflammation and Diabetic Kidney Disease: Why Mitochondria Matter
Posted in GUMC Stories | Tagged diabetes research, kidney research, mitochondrial function, research
(March 12, 2024) — Diabetes mellitus refers to a group of chronic conditions that affect the body’s ability to effectively use sugar, specifically glucose, resulting in a buildup of sugar in the blood. In 2022, the Centers for Disease Control and Prevention estimated that 11.3% of the U.S. population was diabetic and that 38% of adults over age 18 and 49% of adults over 65 were prediabetic, meaning they had higher-than-normal blood glucose levels.
The long-term health effects of diabetes mellitus can be grim. In addition to deteriorating vision, nerve damage and hearing impairment over time, diabetes can also affect larger organ systems. In the U.S., it is the predominant risk factor for cardiovascular and kidney diseases. Diabetics are at increased risk for hypertension, heart attack and stroke; furthermore, one in three diabetic adults have diabetic kidney disease, or DKD.
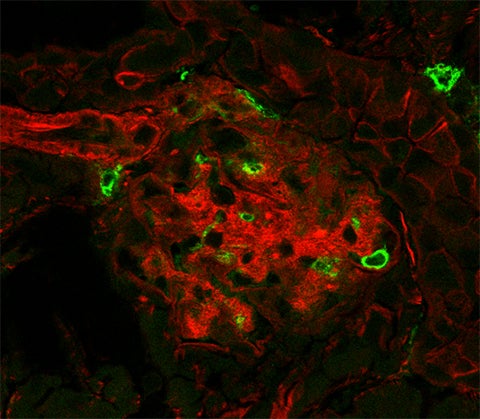
In DKD, prolonged elevated glucose in the blood damages blood vessels and nephrons, the cells in the kidney responsible for filtration. Often occurring in parallel with ailments such as high blood pressure, DKD damages kidneys increasingly over time. A recent study in the Journal of Biological Chemistry demonstrated a potential to mitigate this damage by improving the function of mitochondria, a cellular organelle responsible for maintaining and generating energy.
Komuraiah Myakala, PhD, a research instructor at Georgetown University, uses animal models that mimic Type 2 diabetic disease progression, known as db/db mice, when testing his hypotheses for DKD.

“We have to pick the right model to understand the disease,” Myakala said. “Every metabolic disease is regulated by different signaling pathways; we need to understand, if there is, a causal relationship in kidney disease progression and the signaling proteins involved.”
During the study, db/db and healthy mice were given the supplement nicotinamide riboside, or NR. Also known as vitamin B3, NR is a precursor to the biologically functional form of nicotinamide adenine nucleotide, or NAD+, and can increase its levels within the body. A critical co-enzyme in metabolic processes, NAD+ is ubiquitous to every cell type, where it is essential to mitochondria metabolism and generating cellular energy.
The body naturally produces NAD+. With age, levels decline naturally, and low NAD+ also occurs with conditions such as diabetes, cardiovascular disease and neurological disorders.
“The etiology of kidney disease between diabetes and aging are very different,” Myakala said. “Diabetes is usually a higher-grade kidney disease compared to age alone.”

Inflammation is closely associated with damage to the mitochondria and diabetic kidney disease. Giving NR to the db/db mice reduced inflammation and prevented many of the usual manifestations of kidney decline. For example, levels of blood-protein markers that rise in DKD progression were reduced after NR treatment.
This research helps demonstrate the importance of mitochondrial function in renal disease, particularly in diabetes. Researchers still do not fully understand the mechanisms that link mitochondria and inflammatory disease, and they require further study. This research provides insight, however, into the potential of using supplemental NR to improve mitochondrial function and gives hope for DKD treatment.
Myakala describes his dedication to understanding the mechanisms of kidney disease as “unwavering.” He and his colleagues hope to continue their research as they seek to bridge the gap in understanding that exists between inflammation, mitochondria and kidney disease.
This article was first published by ASBMB Today, the news magazine of the American Society for Biochemistry and Molecular Biology. Read the original.
By Nicole Lynn
Nicole Lynn holds a PhD from UCLA and is an ASBMB Today volunteer contributor.
