Georgetown’s Memory Disorders Program Marks 20th Year
Posted in GUMC Stories | Tagged Alzheimer's disease, clinical trials, mind, neuroscience
(April 12, 2019) — When President Ronald Reagan announced in 1994 that he had Alzheimer’s disease, the man known as the “great communicator” tried his best to convey a sense of optimism.
“I now begin the journey that will lead me into the sunset of my life. I know that for America there will always be a bright dawn ahead,” Reagan wrote in a letter to the American people.
Today, R. Scott Turner, MD, PhD, still shares the late president’s optimism. As director of Georgetown University Medical Center’s Memory Disorders Program, which is celebrating its 20th anniversary, Turner is excited about the developments that lie ahead for research in the field.
“We are too often pessimistic and nihilistic about our progress, or the perceived lack thereof,” he says. “We are doing things today that would be considered science fiction when the program was started.”
From Science Fiction to ‘Everyday Science’
The growing challenges related to Alzheimer’s disease can overshadow the advances that have been made. Six million people are living with the disease in the U.S. By 2050, experts estimate that number will rise to nearly 14 million, for a total of 100 million people worldwide.
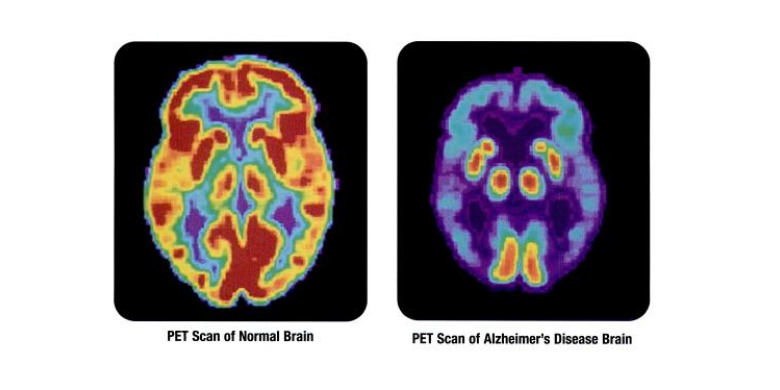
However, while the numbers of those affected by Alzheimer’s disease continue to increase, so too does researchers’ understanding of the disease. Today, scientists have a more expansive understanding of the natural history of the disease, Turner explains, including the discovery of predictive biomarkers that are apparent 10 to 20 years before cognitive decline begins.
“It’s a significant accomplishment that we can identify and enroll older individuals at risk for dementia due to Alzheimer’s — while cognitively intact — into a prevention trial testing an immunotherapy designed to remove amyloid from the brain,” he says.
Although researchers are still evaluating the safety and efficacy of the treatment, Turner believes “this is no longer science fiction, but everyday science.”
Recognizing that there have been repeated disappointments over the last two decades from failed late-stage clinical trials, including the early closure of two studies in March, Turner adds that he and other investigators “have made significant progress in other domains of Alzheimer’s research” that will inform clinical trials going forward.
For example, scientists now understand that slower amyloid clearance with aging sets up a growing imbalance, leading to the concentration of neurotoxic amyloid in the brain. “Some of our current treatment strategies being studied attempt to restore balance between amyloid generation and clearance,” Turner explains.
New Discoveries
Turner joined the Memory Disorders Program in 2008, about a decade after it had been established.
The program’s goals are to provide state-of-the-art clinical care and management, discover improvements in diagnosis, treatment and prevention, and to advance the education of health care providers and trainees in clinical best practices for the management of Alzheimer’s disease and other neurodegenerative disorders
“Similar to watching a child grow into adulthood, day-to-day, even month-to-month changes are imperceptible, but looking back 20 years or more reveals astonishing progress,” Turner says.
As one of the largest Alzheimer’s clinical trials program in the region, the Memory Disorders Program has been at the forefront of finding innovative, evidence-based interventions and mechanisms for Alzheimer’s disease since its founding.
“We led a successful multisite phase 2 trial of resveratrol for Alzheimer’s, reported the first case of Alzheimer’s disease in a person with HIV and launched a phase 2 trial of nilotinib for Alzheimer’s,” Turner recalls. A follow-up phase 1 study of resveratrol for Alzheimer’s with a new formulation (JotrolTM) is now under review for approval and funding.
Over the past two decades, the broader research community has also made progress in the treatment and understanding of Alzheimer’s disease, having identified more than 20 gene variants — including the APOE4 gene — believed to predispose many individuals to the disease.
“These genes point to important disease processes, such as inflammation, and suggest novel therapeutic strategies,” Turner says.
In parallel, new discoveries are advancing the diagnosis and quality of life for individuals with different forms of dementia, including frontotemporal and dementia with Lewy bodies.
Elevated Amyloid as a Managed Disease
Lifestyle factors are increasingly recognized as critical to Alzheimer’s risk, particularly traumatic brain injury, obesity, hypertension and diabetes.
“We recommend that our patients follow a Mediterranean diet and regular exercise to maintain ideal body weight,” says Turner.
In the coming years, he anticipates elevated brain amyloid will become a chronic, manageable disorder similar to hypertension, diabetes and high cholesterol — even HIV and a range of cancers.
“We hope to look back in astonishment as dementia due to Alzheimer’s becomes vanishingly rare,” Turner says. “We seek a world without Alzheimer’s. There is currently no greater unmet need in all of medicine.”
Kat Zambon
GUMC Communications
