Georgetown-led Group Recommends Policy Changes Regarding Sex Diversity in Research
Posted in GUMC Stories
FEBRUARY 20, 2015—A diverse group of experts from academia, industry and advocacy convened by a Georgetown researcher is offering recommendations to the National Institutes of Health (new window) (NIH) regarding how to address the overreliance of male cells and animals used in preclinical studies.
The recommendations come as the federal research institution works to increase the inclusion of female animal models and achieve a balance in the use of male and female cells and animals in lab research.
They were published online Feb. 20 and will appear in the May print edition of FASEB Journal (new window).
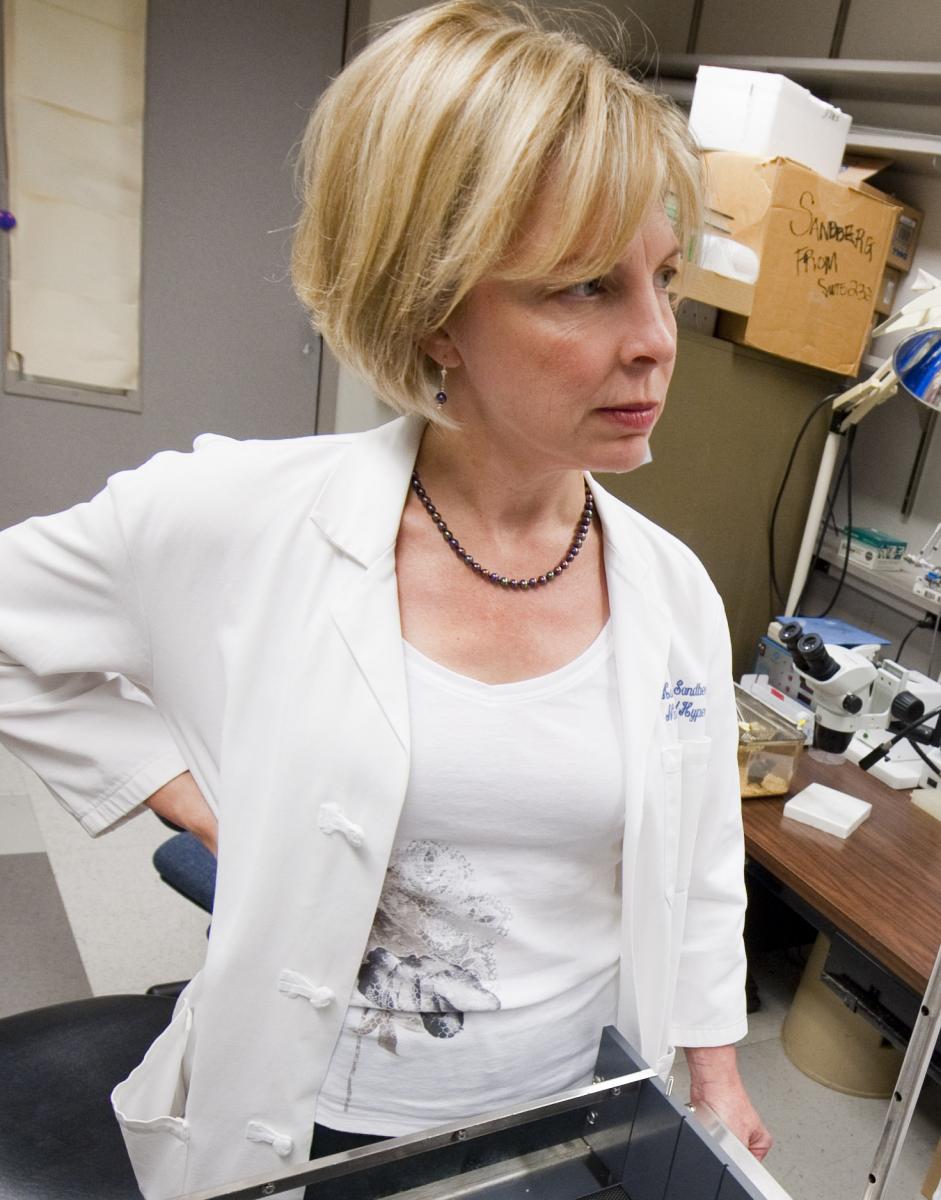
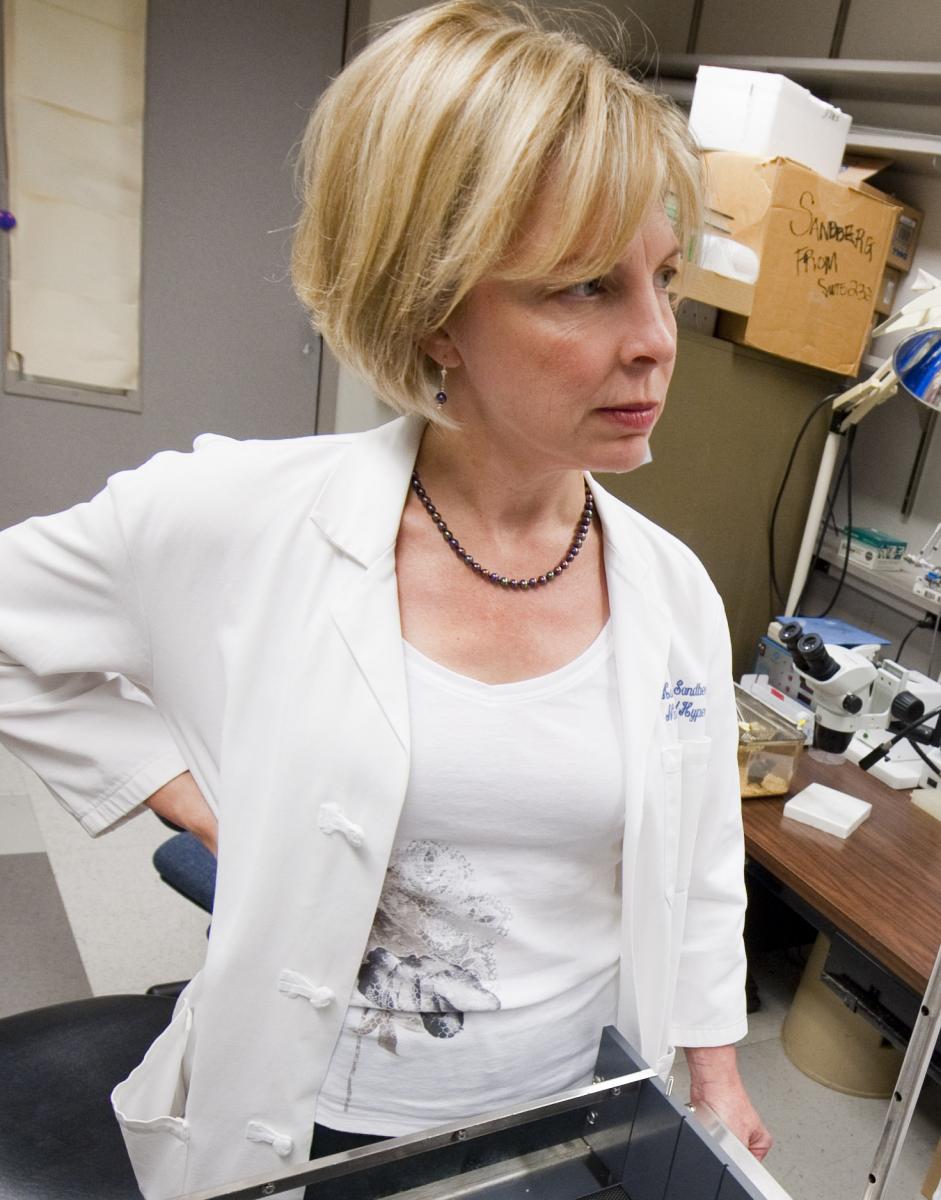
Kathryn Sandberg, PhD (new window), director of Georgetown University Medical Center’s Center for the Study of Sex Differences in Health, Aging and Disease (new window), is the lead author of the recommendations and was instrumental in convening the group..
“The most important message … is the strong recommendation for instituting metrics to measure outcomes in any policy changes designed to address the over reliance of male cells and animals in preclinical research,” Sandberg says. “Without metrics, the NIH will not be able to assess the efficacy of their efforts.”
Staking Out Common Ground
The Georgetown Consensus Conference Work Group, a gathering of basic science, medical and population health researchers, in addition to experts from publishing, industry, advocacy and policy, assembled at Georgetown University Medical Center in September 2014 to work on recommendations that would “aid the NIH as it selects, implements, monitors, and optimizes strategies to correct the over-reliance on male cells and animals in preclinical research,” the authors write.
In May 2014, NIH Director Francis S. Collins, MD, PhD and Janine A. Clayton, MD, director of the NIH Office of Research on Women’s Health, wrote in the journal Nature (new window) that preclinical research “overly relies on male cells and animals.” The NIH announced it would address the problem by enacting policy changes. As part of the Fiscal 2015 appropriations legislation, Congress urged the NIH to move forward with these important changes.
The Georgetown Consensus Group says such policy changes are needed because over-reliance on males in research “obscures key sex differences that could guide clinical studies.”
“Sex is a fundamental biological variable with profound consequences,” the group writes. “Underrepresenting female cells and animals in preclinical research has resulted in a poorer understanding of the biological, physiological and pathophysiological mechanisms in the female compared to the male.”
The group’s four main recommendations to the NIH include:
- Selecting metrics to assess progress in policy changes;
- Implementing educational initiatives that would effect a culture evolution to ensure changes in policy are not superficial and “gamed” in practice;
- Identifying exception criteria for not balancing the sexes in preclinical research; and
- Targeting resources to develop new tools and supporting research that will efficiently reveal sex differences that are important to health outcomes.
Vast Implications for Medicine
Sandberg says sex differences are evident down to the level of cell biochemistry and genes.
“Men and women are not the same, but when they are treated that way, medicine suffers. The Food and Drug Administration (new window) has withdrawn several drugs from the market, and therapeutic doses have been changed, because of the after-market discovery of serious toxic side effects in women,” she says.
One such example is the prescription sleep aid zolpidem, which was re-labeled after the drug was discovered to have more adverse side effects in women, Sandberg notes.
The Georgetown Consensus Group refers to the finding by the U.S. General Accounting Office (new window), that eight of 10 prescription drugs pulled from the U.S. market by the Food and Drug Administration “posed greater health risks for women than for men.”
The group concludes, “The opportunities for drug discovery, new and improved therapeutics and regimens and medical devices arising from research on the impact of biological sex in physiology and pathophysiology are vast. We cannot afford to delay their discovery another day.”
Sandberg says she was pleasantly surprised that such a diverse group of experts was able to arrive at a consensus over their recommendations over “a highly controversial issue.”
“[These recommendations] represent a consensus from diverse interests groups and thus this paper is a strong voice that the NIH can consider as they endeavor to address the over reliance of male cells and animals in preclinical research,” Sandberg adds.
By Karen Teber
GUMC Communications
